PT 861 - The High Risk Infant
Physiological status of the pre-term infant: Part II - Perfusion of the brain
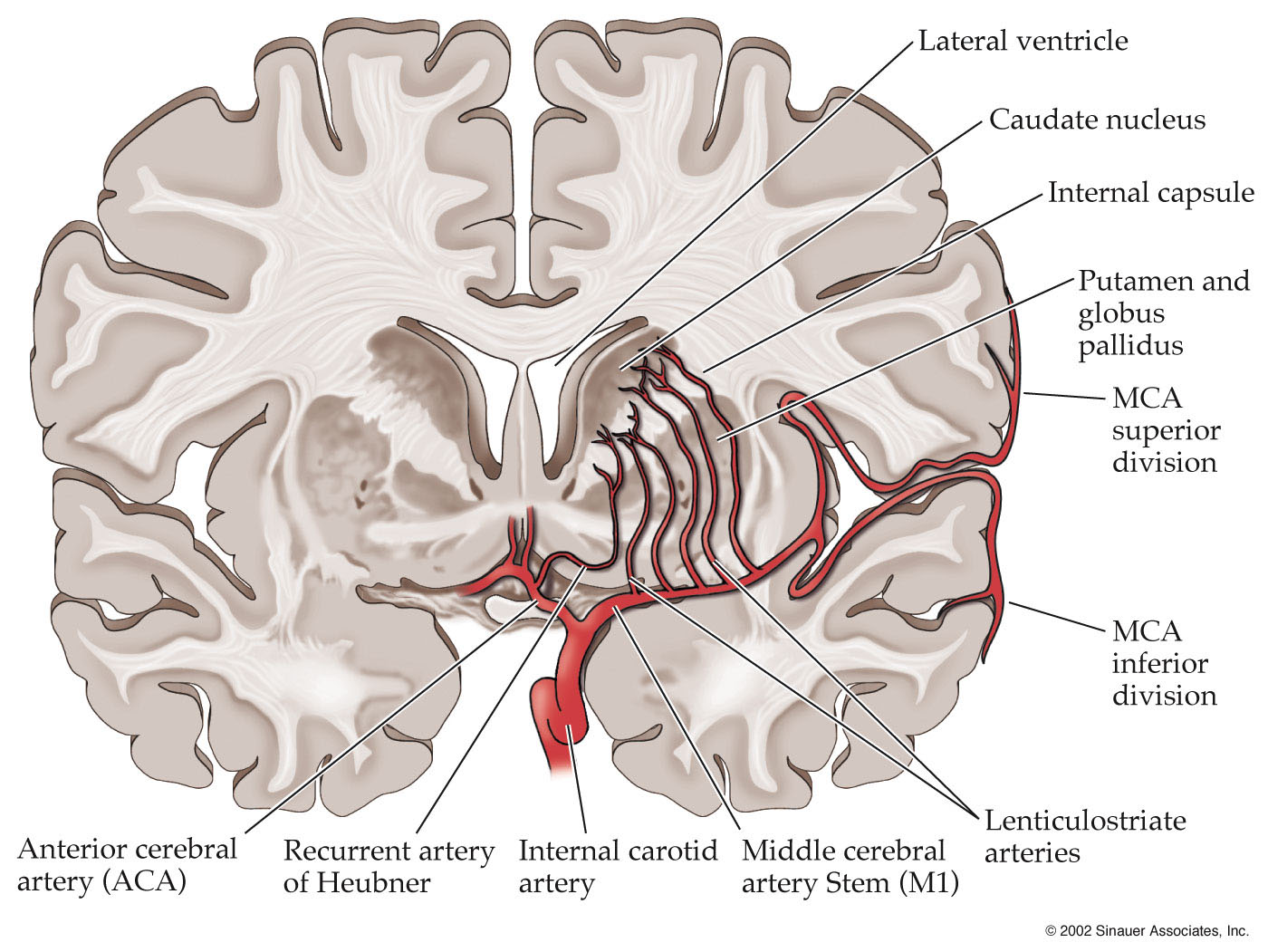
- Pre-term neonates are also at high-risk for ischemic-hypoxic events that can result in infarcts. The areas of the brain that are supplied by the deep branches of the major cerebral arteries are the most susceptible to ischemic events. These areas are shown in the figure below (Blumenfeld).
- One such area is the region of the brain adjacent to the lateral wall of the lateral ventricle, which is perfused by the deep branches of the middle cerebral artery.
What brain structure lies adjacent to the lateral wall of the lateral ventricle?
- These hypoxic-ischemic events are largely related to difficulty of the pre-term infant to
maintain an adequate exchange of O2 and CO2 during ventilation.
- Typically, we find a relative increase in O2
- A relatively higher concentration of O2 that triggers a decrease in blood pressure, which reduces cerebral blood flow.
- The effects of these variations in blood pressure related to ventilatory status are most acute in the small vessels of the deep penetrating branches of the cerebral arteries; these small vessels often collapse with reductions in blood pressure, leading to prolonged periods of ischemia and consequent hypoxia of the surrounding brain tissue.
- The hypoxia results in hypoglycemia of the brain tissue, which results in the production of lactic acid that crosses the blood-brain barrier and increases damage to the brain.
- White matter is highly susceptible to ischemic-hypoxic events as it is being rapidly myelinated during this stage of brain development and, therefore, has a high metabolic demand which increases its relative risk of damage during ischemic events.
- Damage to the white matter tracts of the posterior limb of the internal capsule is called periventricular leukomalacia (or PVL).
- PVL results in a decrease in white matter concentration in the area due to the death of brain cells (see image below).
Cranial MRI (T1-weighted axial image) of an 18-month-old with PVL.
The lateral ventricles are enlarged without hydrocephalus, and the
periventricular white matter is diminished. (Zach et al., 2003).
- Infants born at less than 28 weeks of grestation, and those with a birth weight of less than 1500 g, are also at high-risk for germinal matrix hemorrhage, also known as intraventricular hemorrhage (IVH).
- The germinal matrix is located in the subependyma of the walls of the lateral ventricles, and is highly active between 8 and 28 weeks of gestation, a time when it is producing large numbers of neural and glial cells that will subsequently migrate to populate different cortical regions.
- IVH is associated with significantly higher incidence of hydrocephalus (due to increased intra-ventricular pressure), cerebral palsy, and a range of cognitive and developmental disorders.
- Large hemorrhages can rupture the ventricular wall.

Sagital sonogram of grade 3 germinal matrix hemorrhage shows a subependymal focus
of hyperechogenicity that represents hemorrhage, as well as intraventricular
hemorrhage and hydrocephalus. (Leung et al. et al., 2005)