Equipment tray
 |
Gloves: The rescuer should at all times avoid direct contact with the blood and other body fluids of the patient. If available, gloves should be worn during all airway management procedures. |
 |
Suction: In most resuscitation situations, the patient will either vomit, or at the very least, will have an excess of secretions in their oropharynx. If available, a suction catheter should be included as part of your basic airway equipment. |
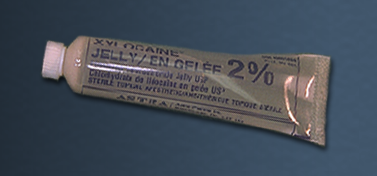 |
Lubrication: The tip of the endotracheal tube should be lubricated prior to insertion. Xylocaine® jelly is a good lubricant because it reduces irritation due to its local anesthetic effect. |
 |
Oropharyngeal airway: In basic airway management, the oropharyngeal airway is used to provide a patent airway to facilitate chest ventilation. In advanced airway management, it can be inserted following endotracheal intubation to act as a bite-block to protect the endotracheal tube. |
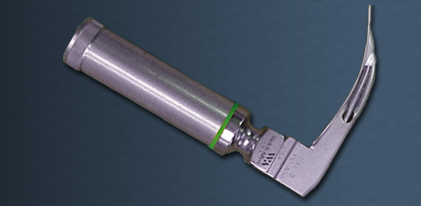 |
Laryngoscope: The laryngoscope handle and blade are used to elevate the tongue and mandible to allow visualization of the cords. The blade can be straight (Miller) or curved (Macintosh). Miller blades are usually reserved for pediatric patients while most physicians use a Macintosh blade for adults. An average sized adult patient would require a #3 Macintosh blade. The blade must be long enough to reach the vallecula (the space between the base of the tongues and the epiglottis). |
 |
Bag-valve ventilator: The bag-valve ventilator is a device designed to ventilate the chest. By attaching an oxygen supply, it can be used to ventilate the chest with a high concentration of oxygen. The bag-valve ventilator can be used with a mask, as in basic airway management, or it can be attached to an endotracheal tube as part of advanced airway management. |
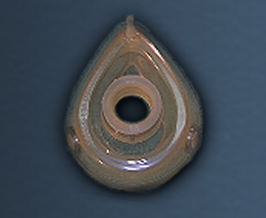 |
Mask: Masks are used to provide a tight seal between the patient's face and the bag-valve ventilator. Masks come in various of sizes. The correct size of mask for a particular patient should provide a tight seal around the mouth and nose. The mask will be needed to ventilate the patient prior to endotracheal intubation. |
 |
Stylet: A stylet can be inserted inside an endotracheal tube to make it more rigid, or to change the shape of the tube. For example, the tip of the endotracheal tube can be bent slightly to facilitate passage through the cords. It is recommended that the stylet be used in all emergency intubations. In this way, if the shape of the tube needs to be modified, the stylet is already in place. The stylet should be lubricated prior to insertion into the endotracheal tube, so that it is easy to remove. |
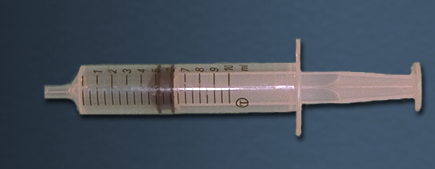 |
Syringe: Endotracheal tubes used in adults have an inflatable cuff near the tip. The cuff, once inflated, is intended to seal the airway from aspiration of oropharyngeal contents, and to prevent air leaks during positive pressure ventilation. A 10 cc syringe should be included on the aspiration tray to inflate the cuff of the tube with 5-10 cc's of air. |
 |
Endotracheal tube: A properly positioned endotracheal (ET) tube will protect the airway from aspiration and greatly facilitate bag-valve ventilation. An adapter at the proximal end allows attachment to a bag-valve ventilator or mechanical ventilator. The internal diameter of the cuff is printed on the side of the ET tube. A 7.5 mm ET tube would be used in an average-sized adult female, and an 8.0 mm ET tube in an average-sized male. The ET tube is also marked in cm to show how far the tube has been advanced into the trachea. |
 |
Tape: Once in place, the ET tube must be secured to avoid inadvertent extubation or migration of the tube down the airway. It is usually taped in place following confirmation of correct ET tube position. |
 |
Stethoscope: The position of the ET tube is confirmed by listening over the lung fields and the epigastrium with a stethoscope. The worst possible outcome of an attempt at endotracheal intubation is unrecognized esophageal intubation. It is absolutely essential that a stethoscope be used to confirm tube positioning by listening over both lung fields and the epigastrium. |
 |
Pillow Correct positioning of the patient's head and neck (neck flexed with extension at the atlanto-occipital joint) will make it much easier to visualize the vocal cords during laryngoscopy. In fact, failed intubation can often be traced to incorrect head positioning prior to laryngoscopy. A pillow or other pad is placed underneath the patient's occiput in order to flex the lower part of the C-spine. The rescuer then extends the head at the atlanto-occipital joint. |